What Is The Difference Between IBS and IBD?
Digestive discomfort is a common concern that many people suffer with, this is often due to conditions like Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD). While the initials look similar, the conditions themselves are distinct, both in terms of symptoms and treatments. Here, we will explore the differences between IBS and IBD, shedding light on their symptoms and available treatment options.
What is IBS:
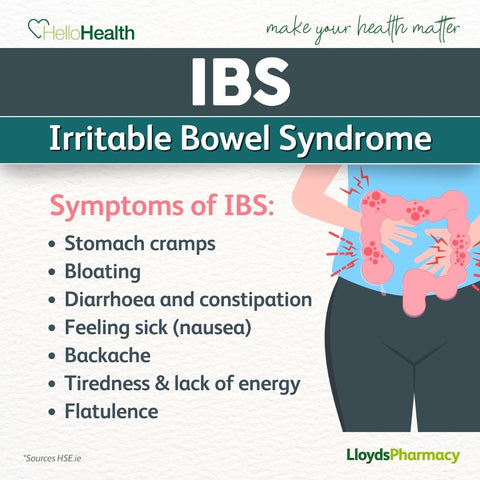
Irritable bowel syndrome (IBS) is a common condition that affects the digestive system. It causes symptoms like stomach cramps, bloating, diarrhoea and constipation. These symptoms tend to come and go over time, and can last for days, weeks or months at a time.
Living with IBS can be quite challenging and can have a big impact on your everyday life. It can be a lifelong problem. Although there's no cure, managing symptoms is possible through dietary changes and medications. These provide relief and improve control over the impact on daily activities.
What are the symptoms of IBS?
The most common symptoms of irritable bowel syndrome are:
- Stomach pain or discomfort – usually worse after eating
- Bloating and gas – stomach can feel uncomfortably full and swollen
- Changes in bowel habits (diarrhoea, constipation, or a combination of both)
- Mucus in the stool
- Relief of symptoms after a bowel movement
What causes IBS?
The exact cause for IBS is unknown but it has been linked to things like:
- food passing through your gut too quickly or too slowly
- oversensitive nerves in your gut
- stress
- family history of IBS
IBS symptoms can be better or worse depending on the day, these are called flare-ups. Flare-ups can happen for no obvious reason but may be triggered by some of the following:
- alcohol
- caffeine
- certain foods, such as spicy or fatty food
- stress and anxiety
Treatment for IBS:
There's no single treatment that works for everyone with irritable bowel syndrome. But there are lots of things that can help if you have been diagnosed with it.
- Dietary Changes:
- Some individuals find relief by adjusting their diet, such as incorporating more fibre or avoiding certain trigger foods.
- Low-FODMAP diet, which restricts fermentable carbohydrates, is often recommended.
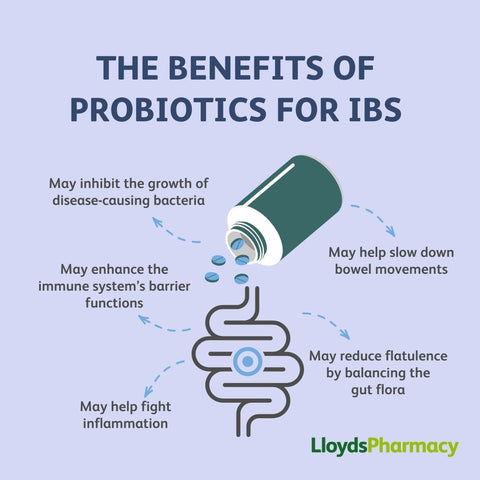
- Medications:
- Antispasmodic medications to relieve muscle spasms in the intestines.
- Probiotics to promote a healthy gut microbiome.
- Stress Management:
- Techniques like relaxation exercises, meditation, and counselling can help manage stress, a common trigger for IBS symptoms.
What is IBD?
Inflammatory Bowel Disease (IBD) is a generic name for a group of chronic inflammatory conditions that affect the digestive tract. These conditions are lifelong and have active and inactive phases. During active phases people can experience increased symptoms of pain, changes in bowel movements and weight loss. There are two main types of IBD, Crohn's disease and Ulcerative colitis:
- Crohn's disease - can cause inflammation anywhere along the gastrointestinal tract and is characterised by patchy inflammation. The main symptoms include pain, diarrhoea and weight loss.
- Ulcerative colitis - causes continuous areas of the colon to be inflamed. The main symptom is bloody diarrhoea, but other symptoms can be present.
Unlike IBS, IBD involves inflammation and may lead to severe complications.
What are the symptoms of IBD?
The most common symptoms of Inflammatory Bowel Disease are:
- Persistent diarrhoea
- Abdominal pain and cramping
- Fatigue
- Weight loss
- Rectal bleeding
- Urgency to have a bowel movement
What causes IBD?
The exact cause for IBD is unknown but it has been linked to things like:
- family history of IBD
- viral or bacterial infection
- factors related to the immune system
- environmental factors
Some evidence suggests that in people with IBD, the immune system reacts too much to regular gut bacteria (called the microbiome). While the immune system is meant to protect the body, in IBD, it becomes too active, causing inflammation.
Treatment for IBD:
Currently there is no cure for IBD. However, there are treatments available that can help to reduce the symptoms:
- Anti-Inflammatory Medications:
- Aminosalicylates to reduce inflammation in the intestines.
- Corticosteroids for short-term relief of symptoms during flare-ups.
- Immunosuppressants:
- Medications to suppress the immune system and reduce inflammation.
- Biologics:
- Targeted therapies that block specific proteins involved in the inflammatory process.
- Surgery:
- In severe cases, surgical intervention may be necessary to remove damaged portions of the intestine.
- Diet & Nutrition:
- A balanced diet of foods from all food groups (grains, dairy, fruits and vegetables, meat and meat substitutes) is recommended to ensure an adequate supply of carbohydrates, proteins and fats.
What are the differences between IBS and IBD:
Given the overlap in symptoms, distinguishing between IBS and IBD can be challenging. However, certain factors can help guide the diagnosis:
- Inflammation:
- IBD involves inflammation, which can be detected through imaging studies, endoscopy, or blood tests.
- IBS does not cause inflammation.
- Structural Changes:
- IBD can lead to structural changes in the intestine visible during imaging or endoscopy.
- IBS does not cause such changes.
- Chronicity:
- IBD is a chronic condition that often requires long-term management, while IBS may have periods of remission.
Understanding the differences between IBS and IBD is essential for getting the right diagnosis and treatment for digestive issues. If you have ongoing digestive symptoms, it's crucial to see a healthcare professional. They can evaluate your condition and create a personalised treatment plan. By learning more about these conditions, we can take proactive steps to improve digestive health and overall well-being.


